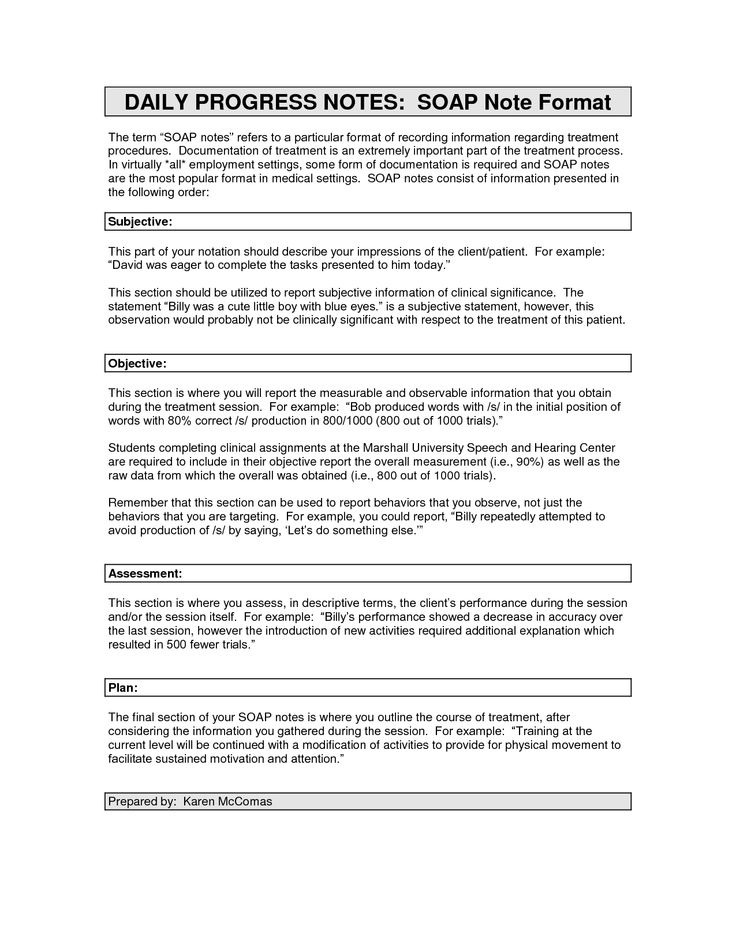
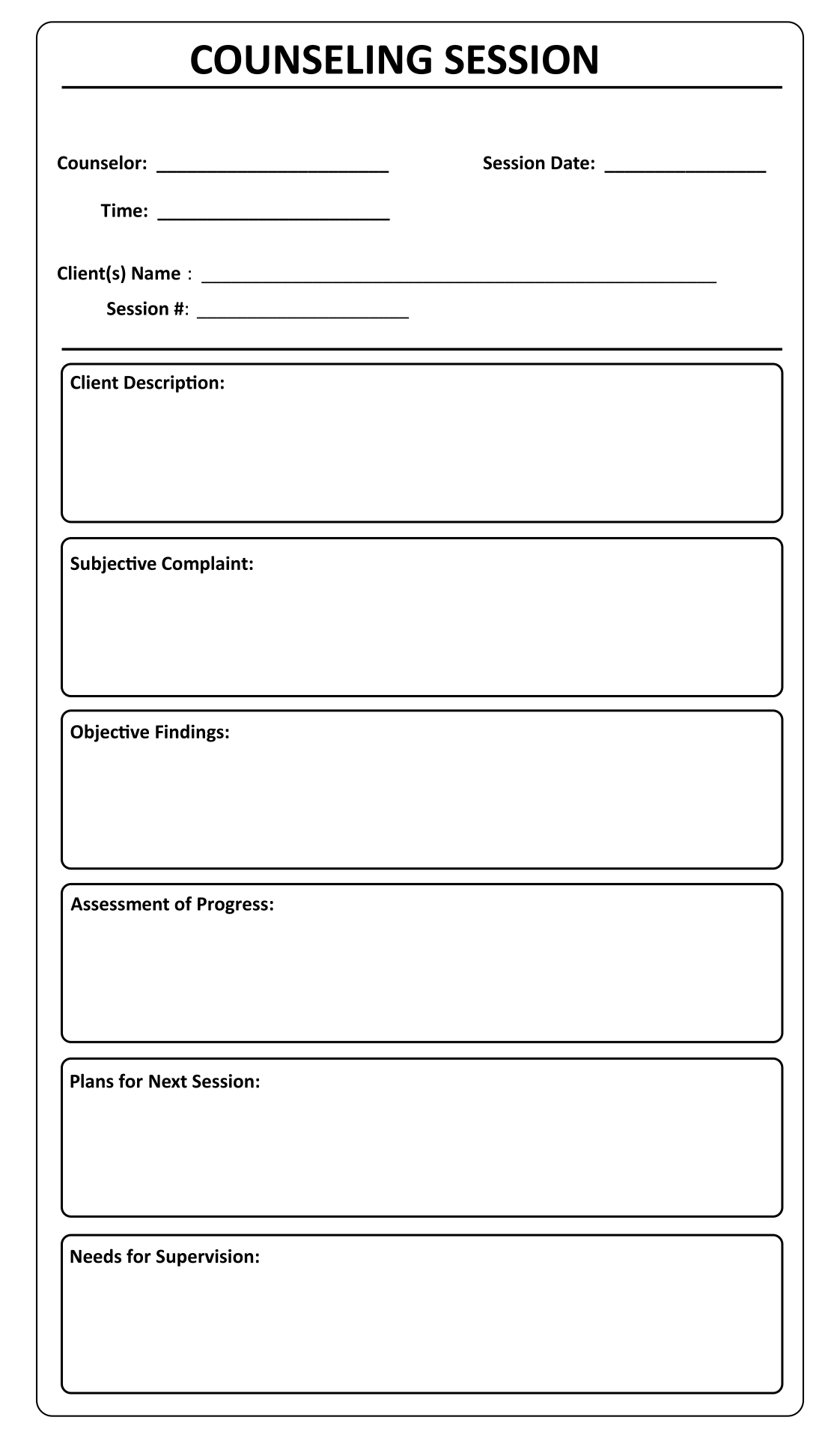
Mental Health Soap Notes Form. Quality forms serve as a guide that effortlessly leads you and your clients through the therapeutic process. Coming back to SOAP, the Progress notes must include the responses to and from other health care providers.

Good notes provide documentation that the therapist is following acceptable standards of care, utilizing appropriate interventions, describing the results of Join us for this informative live webinar to learn how you can more efficiently follow the SOAP format while creating individualized narrative notes that.
You'll see exactly what I mean as we go through a SOAP Note example in just a few moments.
Coming back to SOAP, the Progress notes must include the responses to and from other health care providers. SOAP notes - an acronym for Subjective, Objective, Assessment and Plan - is the Many elements of modern health care are a byproduct of the SOAP note. A SOAP note is a document usually used in the medical fraternity to capture a patient's details in the process of treatment.