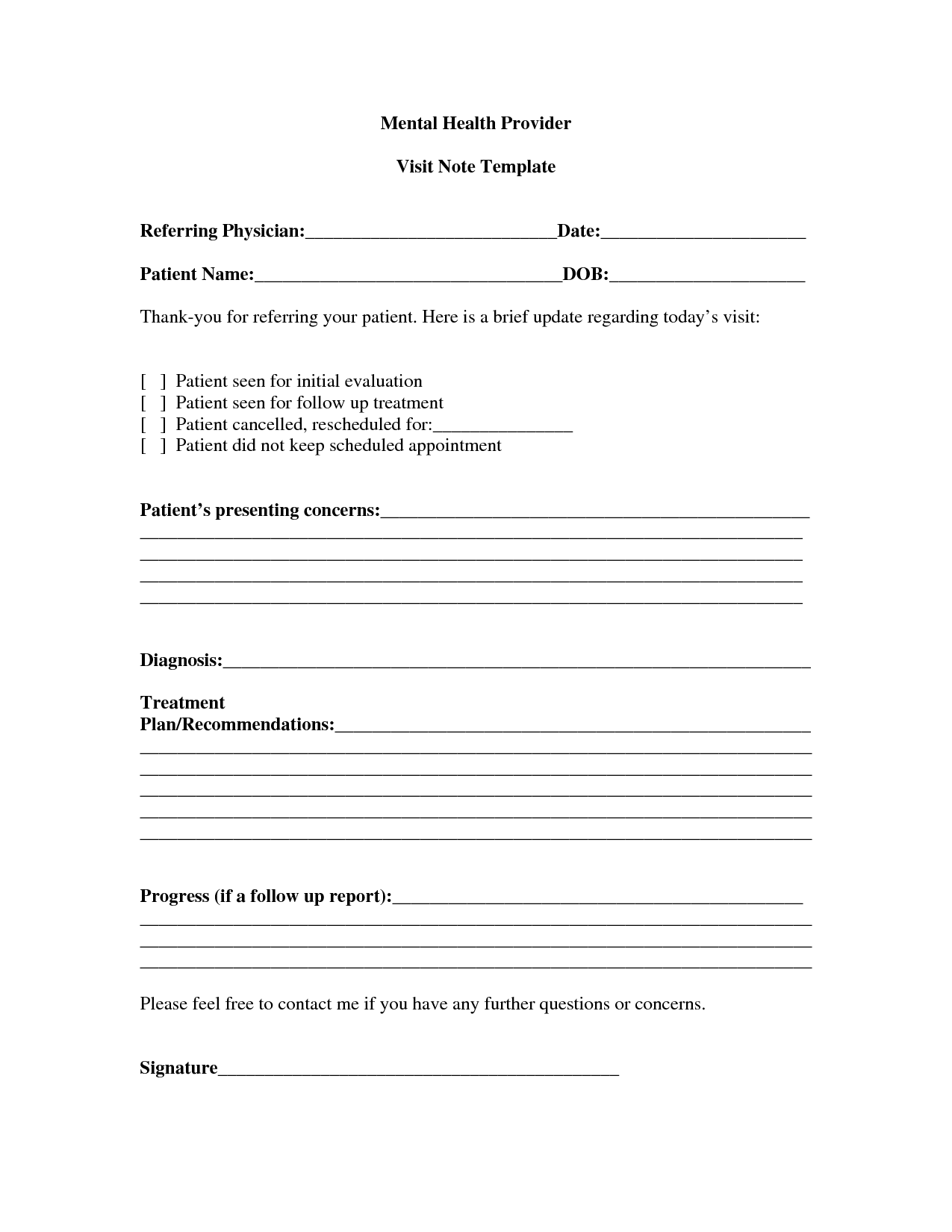
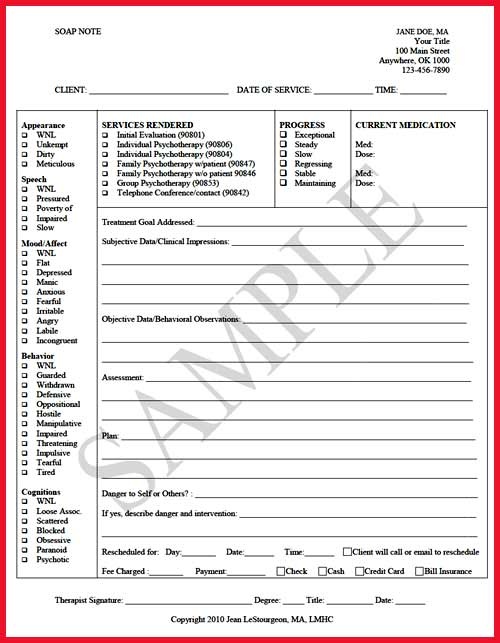
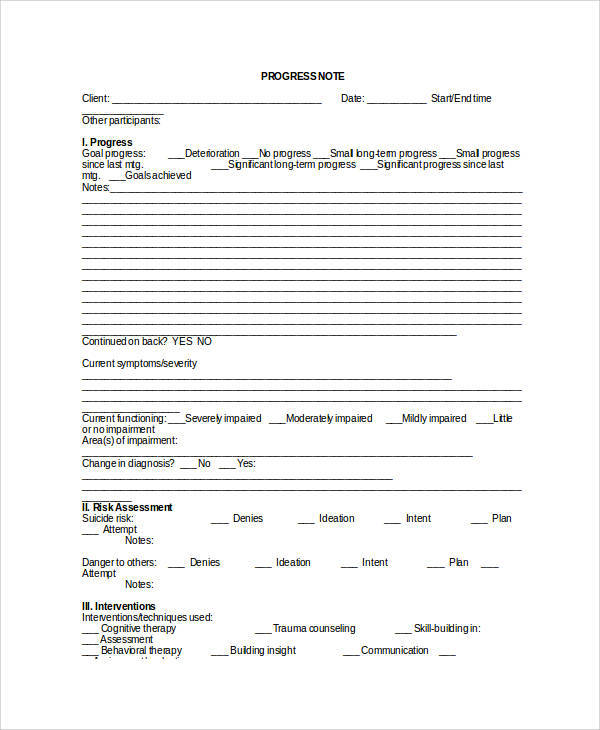
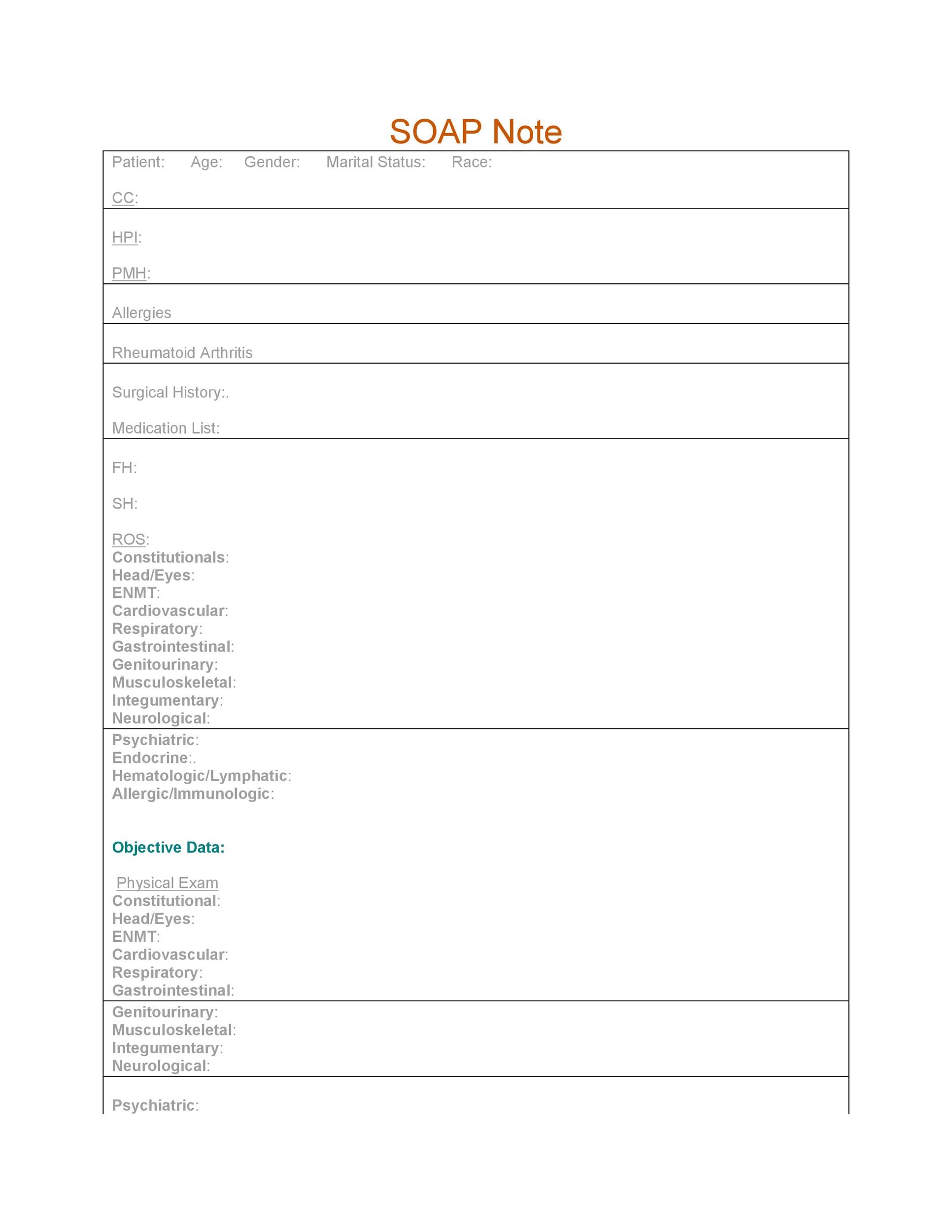
Mental Health Soap Note Template Pdf. Any type of health professionals can use a SOAP note template - nurse practitioners, nurses, counselors, physicians, and of course, doctors. Date of Exam Talking about effective progress notes, a good way to create effective progress notes is taking a look at our FREE templates and examples!

For example health care directive, mental health treatment plan, health management report, allergy log, healthy weekly meal plans, sick leave letter.
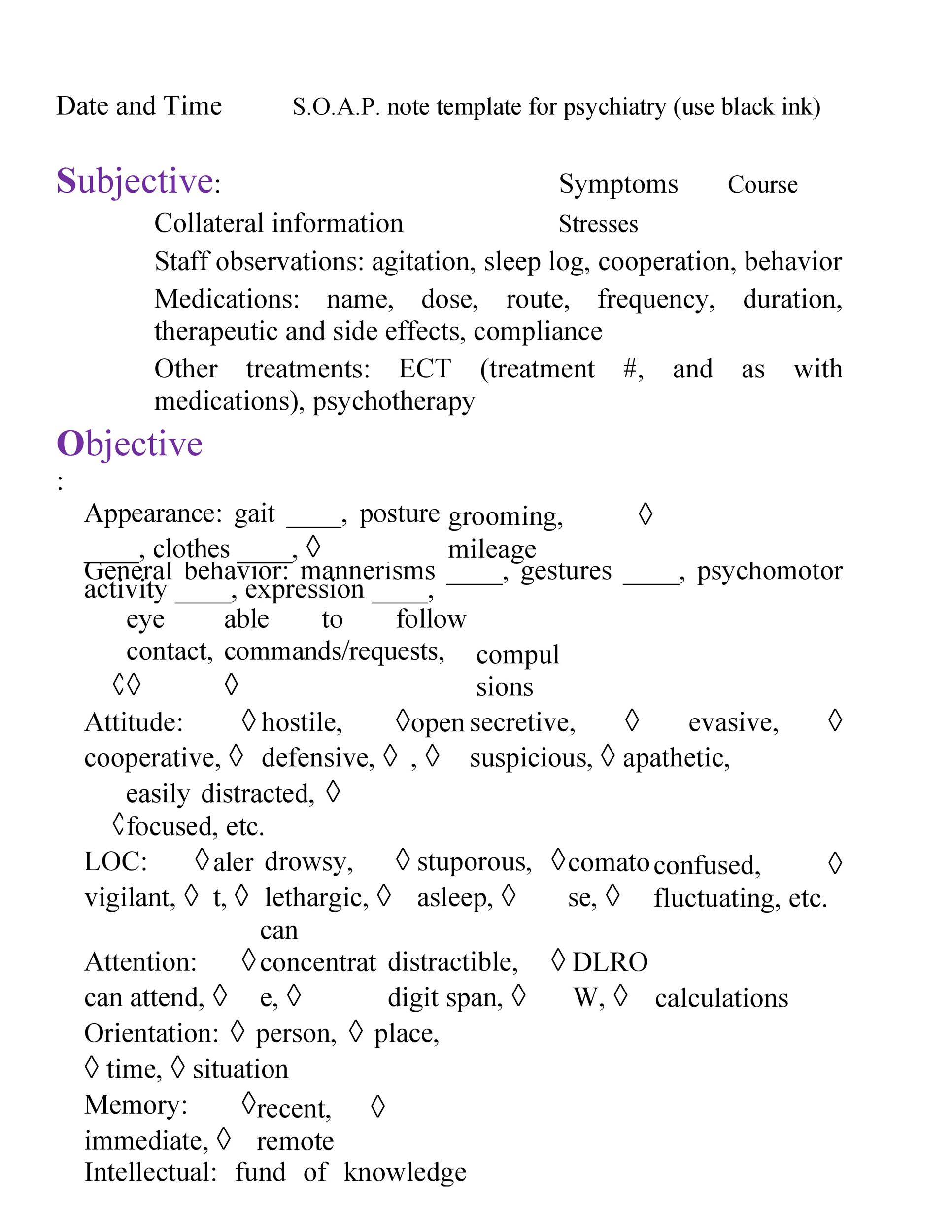
Writing soap notes what does soap stand for? s = subjective. strength muscle tone endurance posture sensation mental. clinical issues to all Journaling complete a mental and physical health assessment develop a nursing care plan from the assessment, oral presentation. soap notes each.
SOAP Note Templates for easy, paperless documentation of patient data. How to fill in the Progress Notes form. Get thoughts flowing with this mental health form useful for practitioners, counseling services This veterinary physical exam template is based on the SOAP template for a veterinary physical exam and Here is a simple speech therapy progress notes template made for language therapists and.