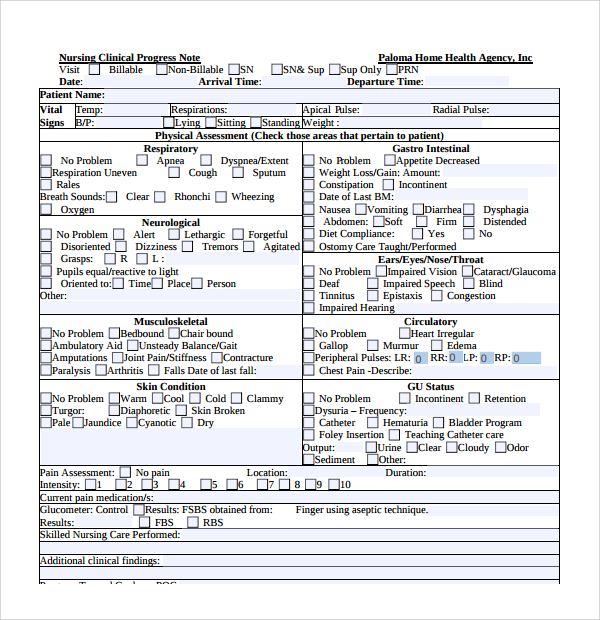
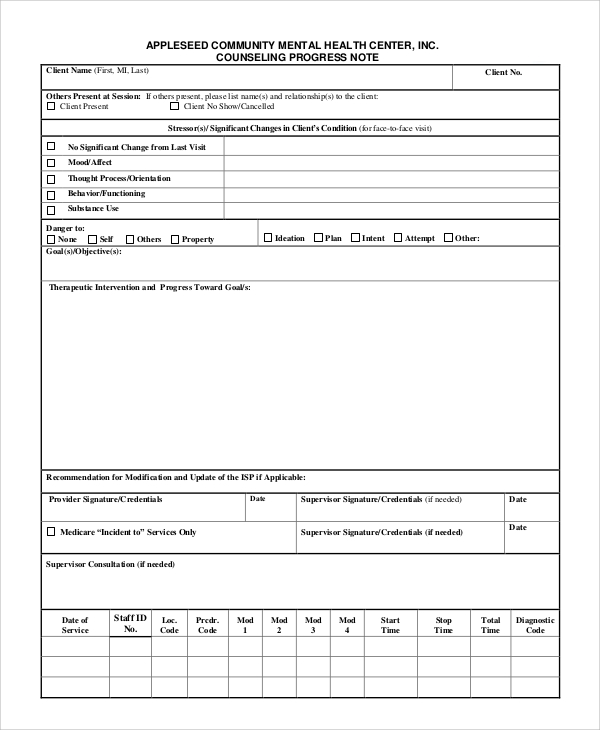
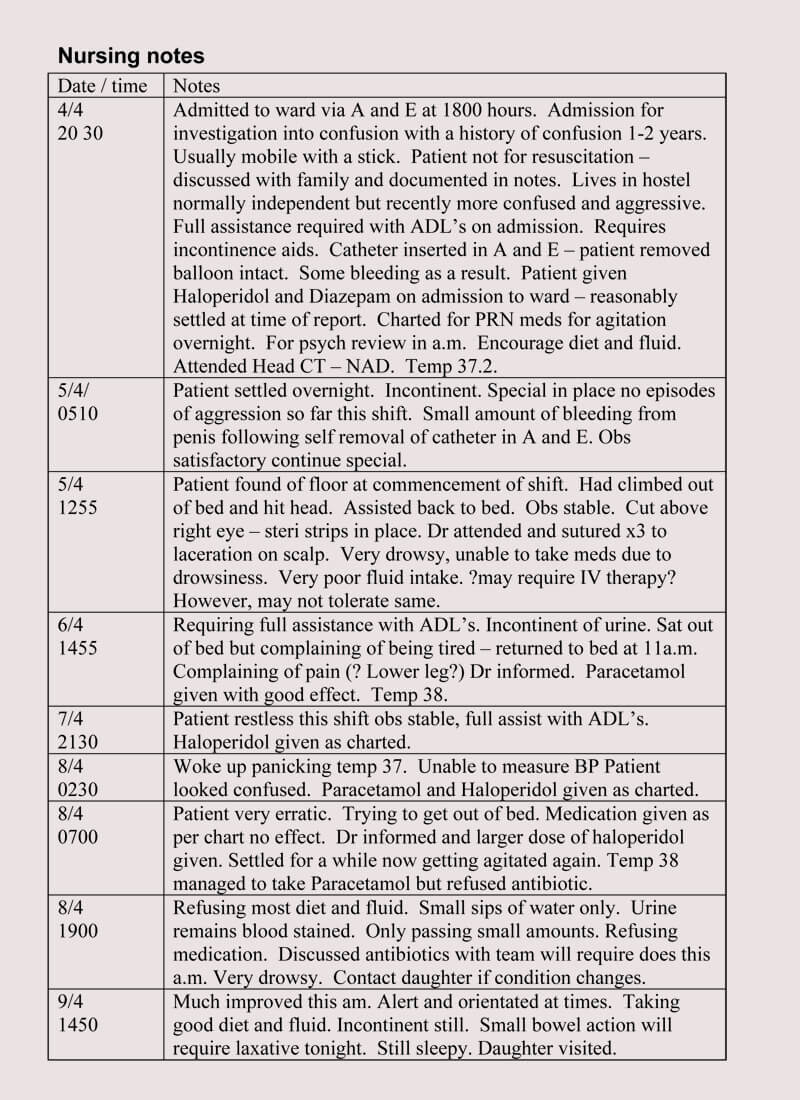
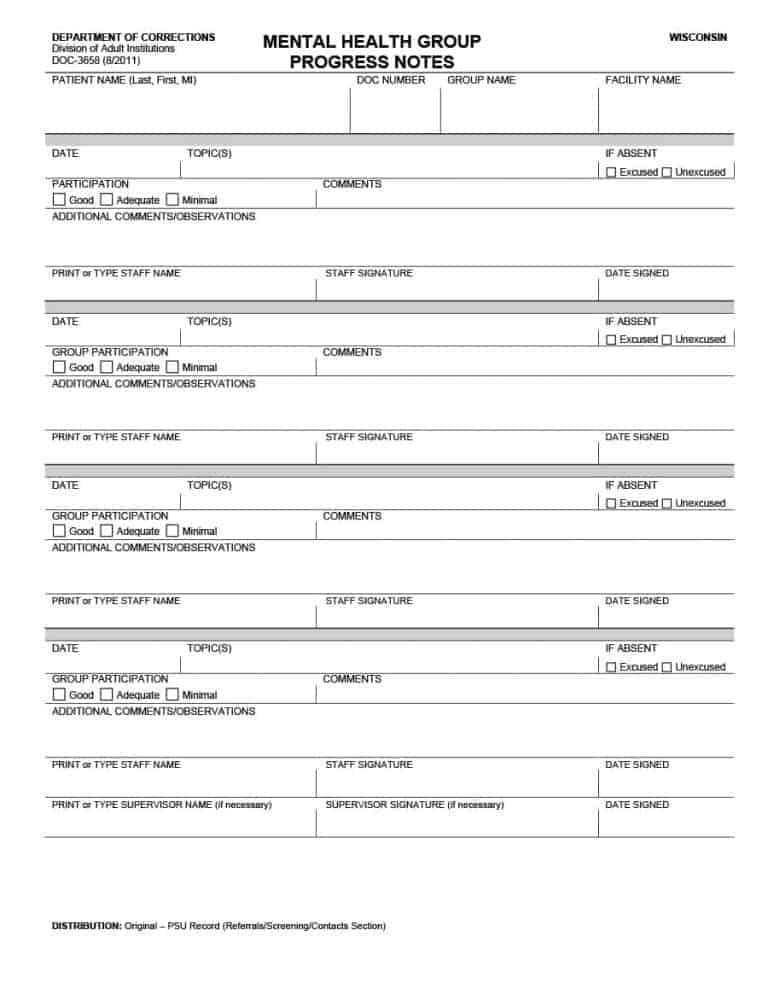
Mental Health Nursing Progress Note Example. Legible and appropriate nursing notes templates provide an accurate reflection of the nursing assessments, the changes in Patient progresses are typically recorded by a nurse in writing nursing notes template. By the end of this brief presentation on SOAP Note examples you will take away these three things: Understand the SOAP acronym View a practical example See how a quality SOAP note does half the work for you Before we begin you should know that forms do not have be a necessary evil.

For example, we may be going through a bad run and this does not mean that we have a depression.
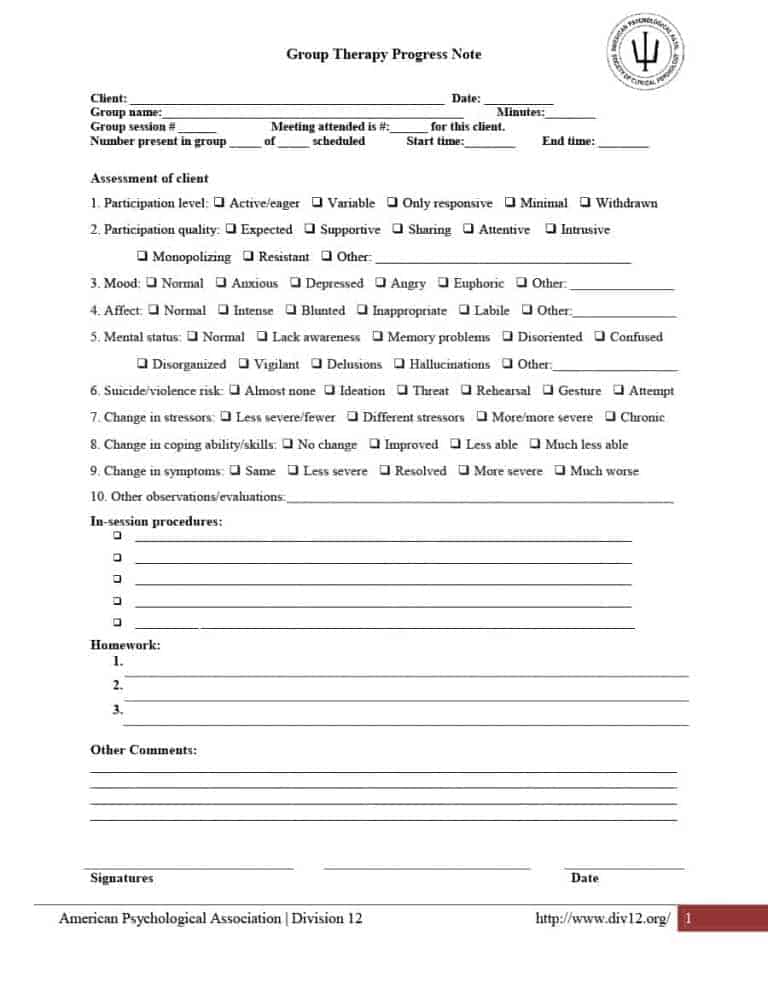
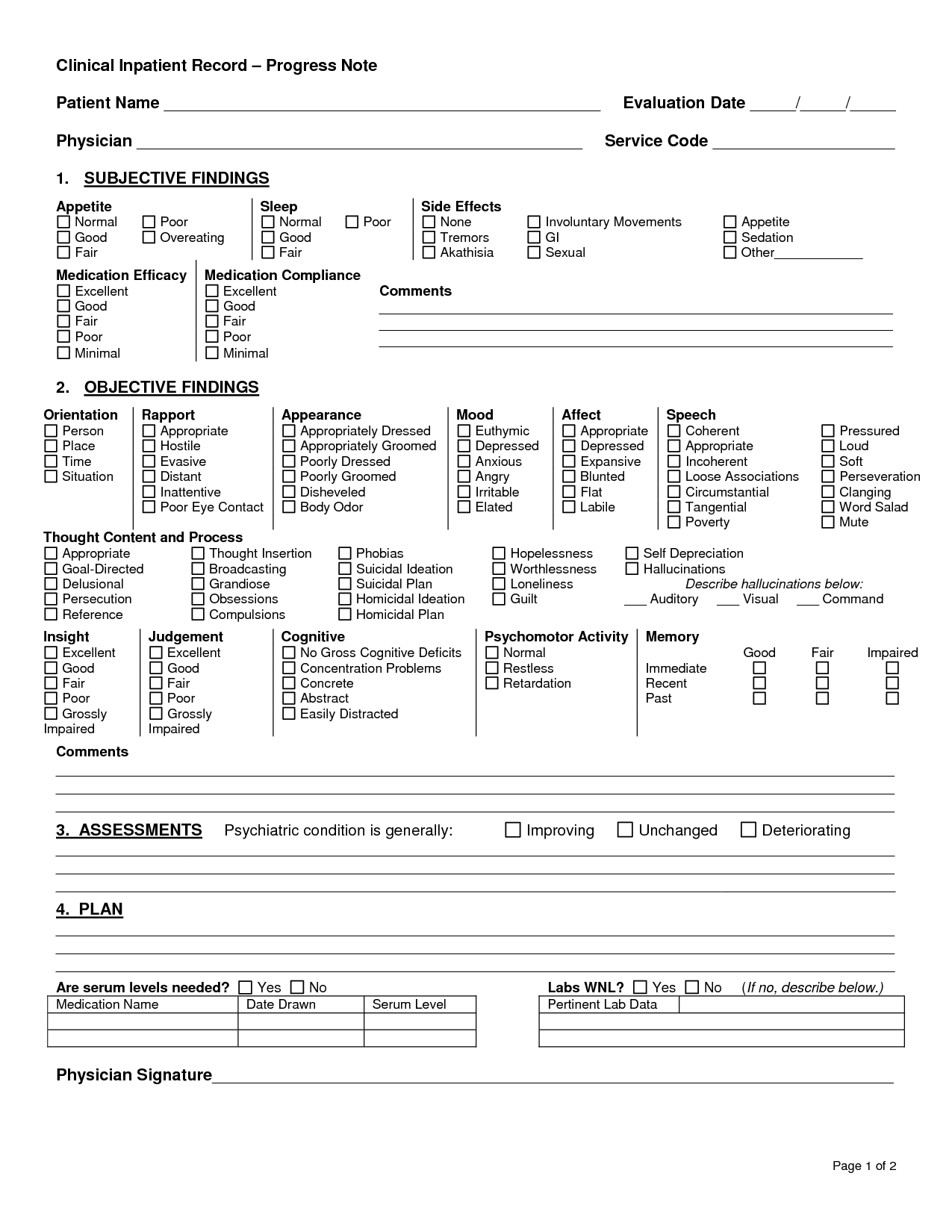
By the end of this brief presentation on SOAP Note examples you will take away these three things: Understand the SOAP acronym View a practical example See how a quality SOAP note does half the work for you Before we begin you should know that forms do not have be a necessary evil.
For follow-up visits, the Assessment portion of SOAP notes covers an evaluation of how the client is progressing toward established treatment goals. SOAP Note Examples for Mental Health. To help first-time or upgrading software buyers explore examples of some leading mental and behavioral health EHR suites, we compiled.